Blood Clots- Prevention of DVT/PE
Deep Vein Thrombosis (DVT) This leaflet has been produced by the hospital Thrombosis and Thromboprophylaxis Group to help explain the management of DVT including the treatment and follow-up arrangements. We hope it answers some of the questions you may have. Who can you contact if you have any concerns or need further information? Your General Practitioner (GP) will be informed that you have had a DVT, and the treatment started by the hospital. If you would like more information or have any questions during working hours, please contact your GP who can contact the Haematology team via the advice and guidance system if required. If you are worried about any new or worsening symptoms that might be associated with your DVT, you should seek medical advice urgently from your nearest Emergency Department or contact NHS 111 (24 hour support). Further information can be found from NHS website (www.nhs.uk) or Thrombosis UK (www.thrombosisuk.org).
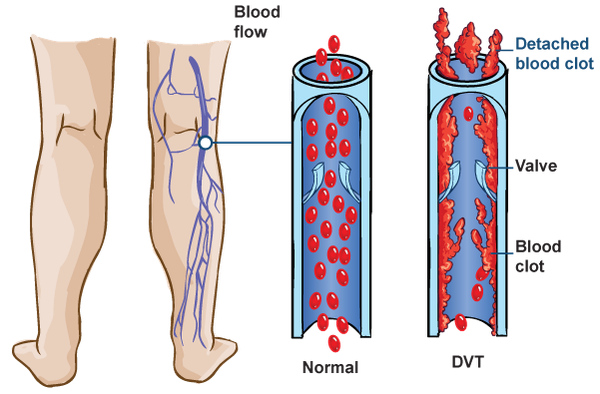
Deep Vein Thrombosis (DVT)
A DVT is a blood clot that has formed in the deep veins (these veins go through the muscle and cannot be seen beneath the skin), usually in the leg or pelvis. A DVT can happen elsewhere in the body e.g. in the calf, behind the knee, in the thigh, arm. Part of the clot may break off (an embolus) and travel up the leg and lodge in your lung(s) causing a pulmonary embolus (PE), which can be serious and life-threatening.
What Causes a DVT?
Sometimes there is no clear reason why a blood clot has formed, but there are associated risk factors such as:
- Pregnancy
- Cancer
- Obesity
- Surgery or prolonged immobility
- Previous or family history of blood clots
- Age of 60 years old
- Oral contraception pill
- Underlying condition of 'sticky blood'
- Smoking
My doctor said the DVT was
- Provoked – usually has an obvious cause or a known contributory factor
OR
- Unprovoked – no clear cause identified
How is a DVT Treated?
Your doctor will prescribe anticoagulation therapy to treat your DVT. The anticoagulant medication, known as a ‘blood thinner’, will prevent the blood clot growing any larger and moving to your lung(s), which may help the symptoms of pain, tenderness and swelling of the leg (usually in the calf); and prevents the blood from clotting as quickly as normal.
Anticoagulant Medication
You will be prescribed an anticoagulant medicine in the form of a tablet, capsule or injection. The choice of anticoagulant medication will be based on various factors e.g. kidney function, body weight, other medications that you are taking.
If you are prescribed an injection, then you, a relative, or a carer will be shown how to give them; and will be provided with a sharps bin to dispose of any sharps (needles) safely. 
Please be aware that some anticoagulants are derived from animal (pig) origin. Please discuss this with your doctor or nurse if this is a concern to you.
My Anticoagulant Medication Details
Indication: Deep Vein Thrombosis (DVT)
Medication: …………………………………………
Recommended Duration: ……………..……………
What should you know about your anticoagulant medication?
To ensure optimal treatment of your DVT, take the anticoagulant medicine exactly as prescribed by your doctor and do not miss any dose(s). You must not stop taking your medication without first talking to your doctor as your risk of blood clots may increase.
Tell your healthcare provider about any other medicines you are currently taking, took recently, or intend to start taking before you start this medication.
Tell your healthcare provider that you are taking an anticoagulant medication before any surgery or invasive procedure (including dental procedure).
Please refer to the manufacturers information leaflet for further information.
What are the main side effects?
Like any medicine, anticoagulants may cause side effects, which will vary from person to person. Anticoagulant medication can increase the risk of bleeding and bruising.
Seek immediate medical advice from your GP or nearest Emergency Department if you experience any of the following:
- Unexplained breathlessness
- Chest pain
- Head injury
- Pink or brown urine

- Red or black, tarry stools
- Coughing up blood
- Vomiting blood, or vomit that looks like coffee grounds
- Excessive bruising or bleeding that does not stop on its own
What Further Investigations or Follow-Up May Be Required?
For patients with uncomplicated DVTs, your case will be reviewed and routinely managed by your GP with no specific follow-up from the hospital.
If further investigations or follow-up appointments are required, you may be contacted with an appointment date. Your GP will then be informed of the outcomes of your treatment.

